Obsessive-Compulsive and Related Disorders
This chapter provides an in-depth exploration of Obsessive-Compulsive and Related Disorders, a group of conditions characterized by persistent, unwanted thoughts (obsessions) and/or repetitive behaviors (compulsions). These disorders, while distinct, share common features of obsessionality, compulsivity, or both, impacting the daily lives and mental health of individuals.
We commence with Obsessive-Compulsive Disorder (OCD), detailing its hallmark symptoms of intrusive thoughts and ritualistic behaviors. The relationship of OCD with other psychiatric conditions such as tic disorders, bipolar disease, depression, and anxiety disorders is examined, along with neuroimaging findings like increased activity in the caudate nucleus.
Body Dysmorphic Disorder (BDD) is then discussed, highlighting its characteristics of excessive preoccupation with perceived physical flaws. The chapter also delves into Hoarding Disorder, describing its manifestation, associated conditions, and the importance of a supportive treatment approach. Trichotillomania (Hair-Pulling Disorder) and Excoriation (Skin-Picking) Disorder are explored next, detailing their clinical presentations, associated psychiatric comorbidities, and therapeutic strategies.
Overall, this chapter offers a comprehensive guide to understanding, diagnosing, and managing obsessive-compulsive and related disorders, providing residents with the necessary tools to approach these complex conditions with confidence. The content of this chapter is designed to equip psychology residents with the knowledge necessary for the In-service exam and ABPN Psychiatry Boards exam, focusing on diagnosis, clinical features, and treatment modalities.
Obsessive-compulsive disorder
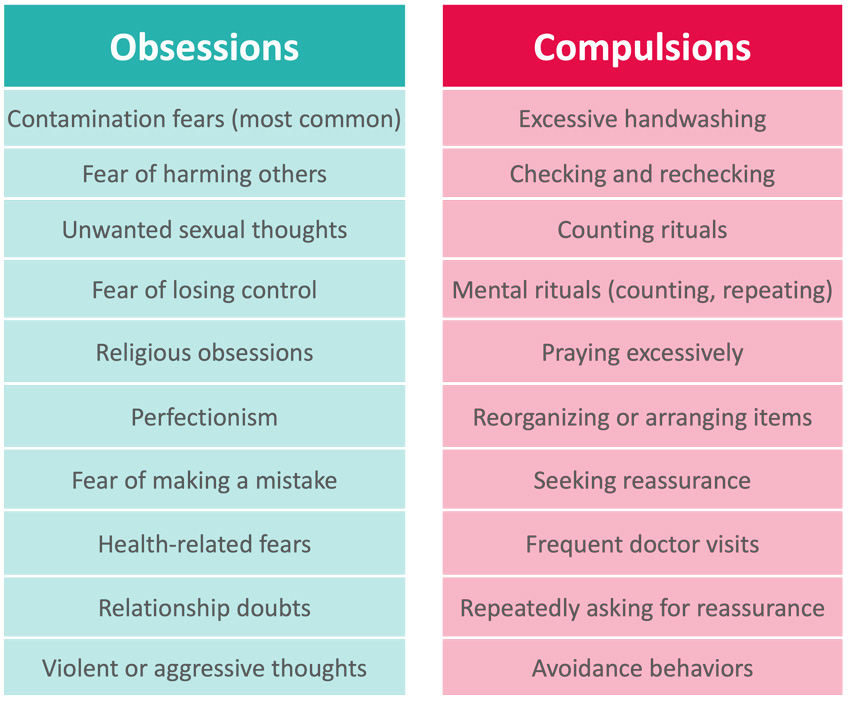
- Characterized by the presence of intrusive, distressing, and repetitive thoughts, images, or urges (obsessions) and repetitive behaviors or mental acts aimed at reducing distress associated with obsessions (compulsions).
- Patients spend over an hour on obsessions and compulsions a day.
- Other common character traits of those with OCD include an exaggerated sense of responsibility and perfectionism.
- May fear that if compulsions are not completed bad things will happen and that completing these tasks is “important”.
- The severity of symptoms can be monitored by the Yale-Brown Obsessive Compulsive Scale (Y-BOCS).
- Symptoms present in childhood to early adulthood.
- Patients are often aware and have significant insight into their irrational beliefs and behaviors.
- Associated with anxiety disorders, depression, tic disorders, bipolar disease, anxiety disorders, social phobia, and substance abuse.
- Symptoms are felt to be secondary abnormalities in the cortico-striato-thelamo-cortical circuits.
- PET scans in a patient with OCD can show increased activity in the caudate nucleus.
- Treatment:
- Cognitive behavioral therapy with exposure and response prevention.
- Antidepressants approved by the FDA for the treatment of OCD:
- Fluvoxamine (adults and children 8 years and older)
- Paroxetine (adults only)
- Clomipramine (adults and children 10 years and older)
- Fluoxetine (adults and children 7 years and older)
- Sertraline (adults and children 6 years and older)
- SSRIs are preferred over clomipramine
- CBT and pharmacotherapy can be given in combination for those with severe symptoms.
- Cingulotomy and deep brain stimulation can be considered a last-resort treatment for refractory cases.
- This has ‘limited humanitarian’ FDA approval.
Log in to view the remaining 60-90% of page content!
New here? Choose an account!
1 Month Plan
Full Access Subscription-
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
3 Month Plan
Full Access Subscription-
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
1 Year Plan
Full Access Subscription-
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank