Depressive Disorders
This chapter aims to equip psychiatry residents with a thorough understanding of depressive disorders. It offers a comprehensive overview including detailed diagnostic criteria, treatment options, and theoretical perspectives, while also providing a holistic understanding of these complex conditions. Particular attention is focused on pharmacology, as many of the medications used for depressive disorders are also used for various other psychiatric and neurologic issues.
Authors: Michael Franklin, MD & Brian Hanrahan, MD
Persistent Depressive Disorder (Dysthymia)
- Characterized by depressed mood more days than not for at least two years.
- Patients may never be completely symptom-free for more than 2 months at a time.
- Children and adolescents can meet diagnostic criteria if symptoms are present for at least one year.
- Additional symptoms include feelings of hopelessness, poor sleep (insomnia or hypersomnia), decreased or increased appetite, low energy, low self-esteem, and poor concentration.
- Treatment: Antidepressants plus psychotherapy.
- More refractory to treatment than major depressive disorder.
Tip:
Use the mnemonic HE'S 2 SAD to remember the criteria for persistent depressive disorder:
- H - Hopelessness
- E - Energy low
- S - Self-esteem
- 2 - 2 years of symptoms
- S - Sleep decreased
- A - Appetite poor
- D - Difficulty making decisions
Premenstrual Dysphoric Disorder
- Characterized by significant mood disturbances in the majority of menstrual cycles in the final week before the onset of menses (luteal phase).
- Symptoms improve with the start of menses and are minimal after menses.
- Symptoms can worsen during menopause and improve after menopause.
- Mood disturbances must include one of the following: Affective lability, irritability, depression, or anxiety.
- Other possible symptoms include poor concentration, low energy, and poor appetite.
- SSRIs can be used and can even be effective if given only during the luteal phase.
- Hormonal contraceptives can help reduce symptoms
Substance/Medication-Induced Depressive Disorder
- Characterized by prominent depressed mood with evidence that it is in the time course of medication or substance intoxication or withdrawal.
- Examples:
- Alcohol intoxication and withdrawal
- Opioids withdrawal
- Stimulant withdrawal
- “Crash” after stimulant intoxication can induce a period of depression, fatigue, insomnia.
- Sedatives/Hypnotics withdrawal
- Rebound anxiety and insomnia are also common.
- Chronic cannabis use
- Risk may be higher in those with existing mood disorders.
- Anabolic Steroid withdrawal
- Possible manic or depressive symptoms during use as well.
- Interferons
- Often induce neuropsychiatric side effects including possible long-lasting depression and suicidal ideation.
Note
Note: L-dopa, anticonvulsants, antihypertensives, antimalarials, isotretinoin and other medications rarely linked to increased depression risk.
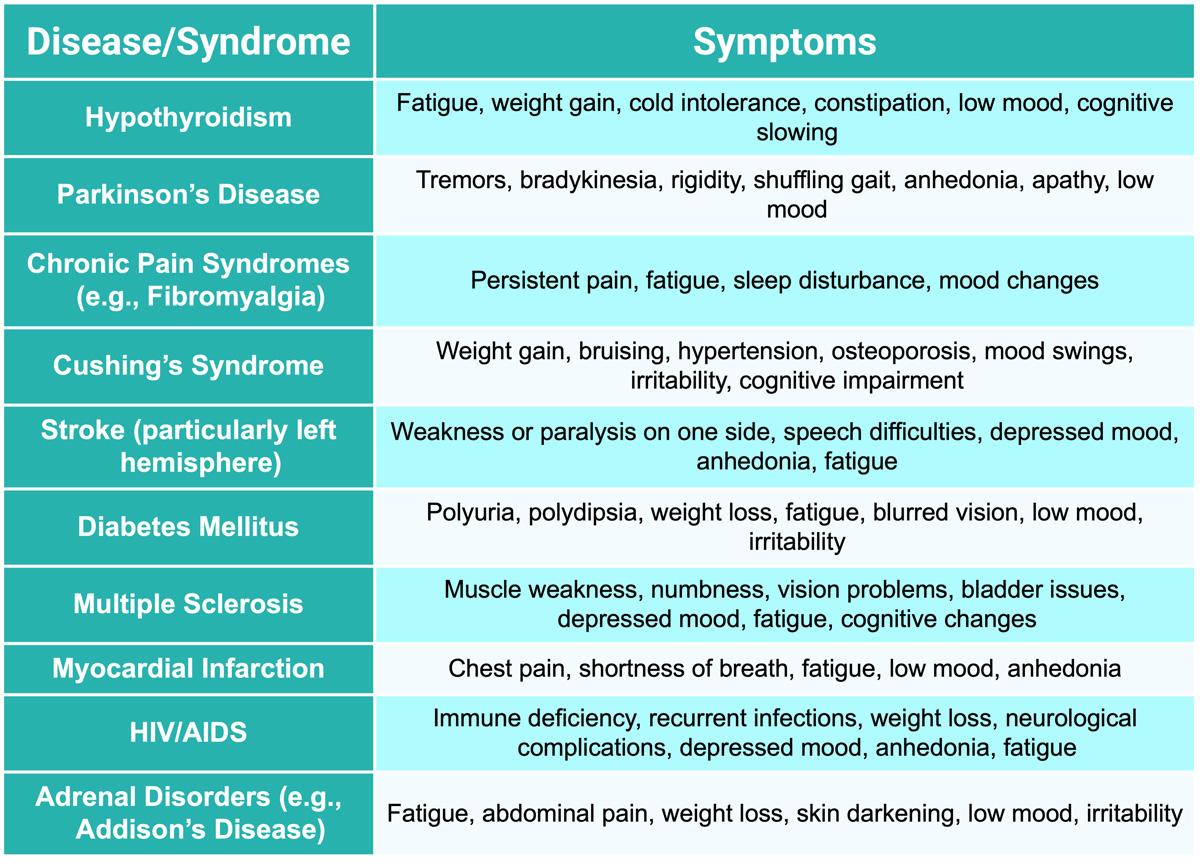
Depressive Disorder due to other Medical Condition
- Characterized by a prominent depressed mood with evidence that it is caused directly by the pathophysiologic process of another medical illness.
Log in to view the remaining 60-90% of page content!
New here? Choose an account!
1 Month Plan
Full Access Subscription
$68
$
48
49
1 Month -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
3 Month Plan
Full Access Subscription
$159
$
73
49
3 Months -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
1 Year Plan
Full Access Subscription
$446
$
195
49
1 Year -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
Popular
Loading table of contents...
Loading table of contents...