Central Nervous System Disorders
The central nervous system encompasses the brain, brainstem, and spinal cord. There are a large number of disorders affecting the central nervous system, but we have distilled the most high-yield content for the PRITE® and psychiatry board exam here! Review the chapter and then test your knowledge with flashcards and practice questions!
Vascular diseases
Transient ischemic attack (TIA)
- Defined as a transient episode (<24 hours) of neurologic dysfunction caused by focal ischemia, without acute infarction.
Ischemic Stroke
Stroke subtypes
Large-artery atherosclerosis
- The most common cause of ischemic stroke in the world.
- Patients will have either significant stenosis or occlusion of a major brain artery or branch cortical artery.
Cardioembolism
- The most common cause of ischemic stroke in the United States.
- Patients can present similarly with comparable imaging to those with large-artery atherosclerosis but will have a cardiac source for the embolic phenomenon.
- Sources of cardioembolism: Atrial fibrillation, mechanical heart prosthetic valve, left atrial or ventricular thrombus, recent myocardial infarction, dilated cardiomyopathy, valvular heart disease, structural heart defects, tumors, etc.
Lipohyalinosis/small-vessel disease
- Also known as lacunar strokes
- Risk factors: Hypertension, diabetes, and smoking.
Stroke of Other Determined Etiology
HYPERCOAGULABLE STATES AND COAGULOPATHY
Examples: Factor V Leiden, antiphospholipid antibody syndrome, protein S/C deficiency, prothrombin gene mutation, antithrombin III syndrome, sickle cell disease, thrombotic thrombocytopenic purpura (TTP), polycythemia, hyperhomocysteinemia, MTHFR gene mutations, and malignancy.
- CENTRAL NERVOUS SYSTEM (CNS) VASCULITIS
- Caused by a diverse spectrum of diseases that typically involves the gray/white matter junction.
- ARTERIAL DISSECTION
- Dissections are due to a tear of the vessel wall intima leading to the formation of a false lumen.
- Symptoms can include head/neck pain and Horner syndrome. Ischemic events occur due to thromboembolism formation and less often cerebral hypoperfusion.
- A common cause of stroke in the young. Should be considered in a patient with a history of neck trauma, chiropractic neck manipulation/high-velocity neck injury, or connective tissue disease (fibromuscular dysplasia, Marfan syndrome, Ehlers-Danlos syndrome).
- PATENT FORAMEN OVALE (PFO)
- PFO’s shouldn’t be considered as an etiology for stroke unless a patient presents with a cryptogenic embolic stroke.
- HYPOPERFUSION
- Hypoperfusion can cause watershed regions between major vascular territories to become ischemic.
- MITOCHONDRIAL ENCEPHALOPATHY, LACTIC ACIDOSIS, AND STROKE-LIKE EPISODES (MELAS)
- MELAS is a mitochondrial disease caused by a mitochondrial DNA mutation to the gene MT-TL1.
- Most common mitochondrial disease
- Symptoms of ischemic strokes, seizures, and headaches present before the age of 40.
- Diagnostic testing will reveal elevated cerebral spinal fluid lactate levels, serum lactic acidosis, and ragged red fibers on muscle biopsy
- TRAUMA
- DRUGS/TOXINS
Acute Treatment of Stroke
Tissue plasminogen activator (tPA)
- Works by transforming plasminogen into plasmin, leading to fibrinolysis of the clot
- Can be given within 4.5 hours from the time of last seen well.
Tenecteplase (TNK)
- A modified form of human tissue plasminogen activator (tPA)
- Ischemic stroke or severe head trauma in the previous three months
- Previous intracranial hemorrhage
- History of intracranial neoplasm
- Gastrointestinal malignancy or hemorrhage in the previous 21 days
- Intracranial or intraspinal surgery within the previous three months
- Subarachnoid hemorrhage
- Blood pressure ≥185 mmHg systolic or ≥110 mmHg diastolic
- Active internal bleeding
- Infective endocarditis
- Aortic arch dissection
- Acute bleeding diathesis, including but not limited to conditions defined as “hematologic”
- Platelet count <100,000/mm
- Current anticoagulant use with an INR >1.7, PT >15 seconds, or aPTT >40 seconds
- Low molecular weight heparin (LMWH) use within 24 hours for PE or DVT (not at prophylactic doses)
- Direct thrombin inhibitor, direct factor Xa inhibitor, or glycoprotein IIb/IIIa receptor inhibitor use
- Evidence of hemorrhage on CT head
- Extensive regions of hypodensity consistent with irreversible ischemic injury
- Minor or rapidly improving symptoms
- Serum glucose <50 mg/dL
- Serious trauma or major surgery in the previous 14 days
- History of gastrointestinal bleeding or genitourinary bleeding
- Seizure at stroke onset
- Pregnancy
- Arterial puncture at a noncompressible site in the previous 7 days
- Large (≥10 mm), untreated, unruptured intracranial aneurysm
- Intracranial vascular malformation
Note: Pregnancy is not a contraindication for tPa or tenecteplase
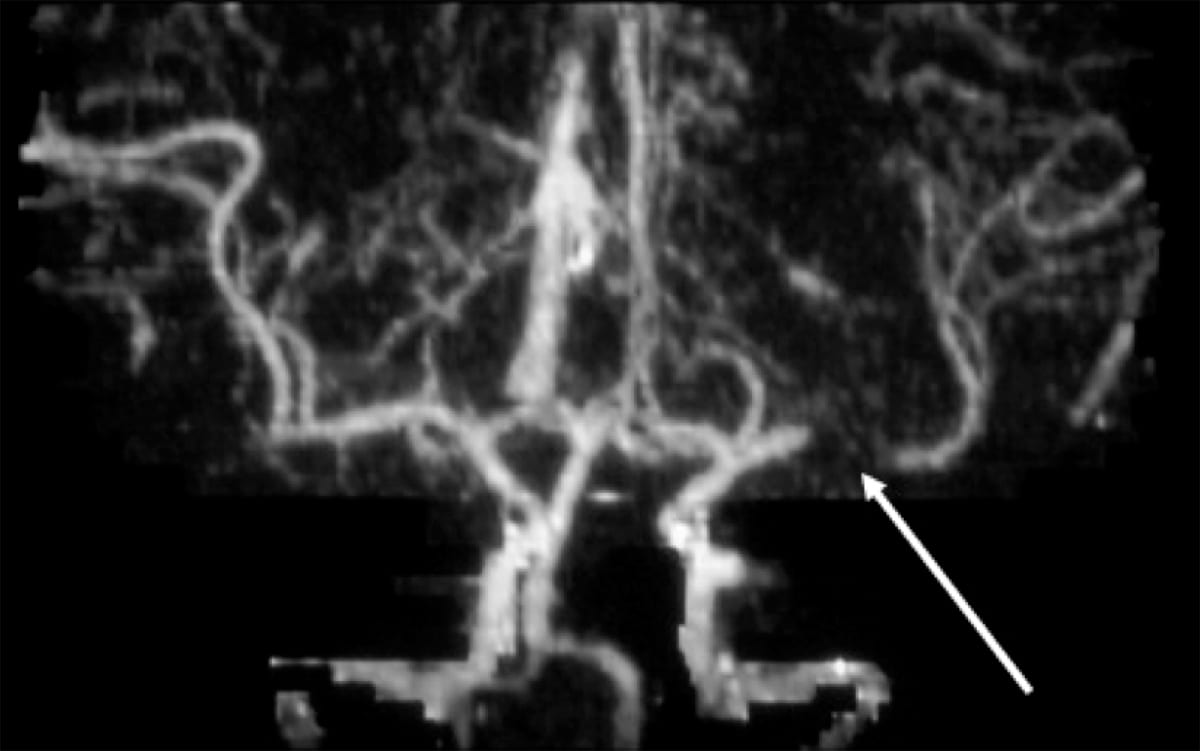
Intra-arterial therapy (IAT)
- Patients who undergo IAT should have a large vessel occlusion seen on CTA/MRA.
Secondary stroke prevention
- Includes management of major risk factors such as diabetes, hyperlipidemia, hypertension, tobacco use, and utilization of antiplatelet and/or anticoagulation therapy.
Antiplatelets
- Aspirin:
- Mechanism of action: Irreversible cyclooxygenase (COX-1 >> COX-2) inhibition.
- Clopidogrel: Adenosine diphosphate (ADP) receptor inhibitor.
- Clopidogrel is converted to its active metabolite by the cytochrome P450 system.
- A minority of patients with CYP genetic variants are poor metabolizers of clopidogrel, and thus will have an inadequate antiplatelet function (i.e. inadequate conversion of clopidogrel to its active form).
- Clopidogrel is converted to its active metabolite by the cytochrome P450 system.
- A combination of aspirin and clopidogrel is more effective than monotherapy for secondary stroke prevention after ischemic stroke in the first 90 days after stroke with intracranial atherosclerosis, and likely for TIAs/mild strokes as well.
- Other rarely used antiplatelet medications include glycoprotein IIB/IIIA inhibitors (abciximab, eptifibatide, tirofiban) and adenosine reuptake inhibitors (dipyridamole).
Anticoagulants
- Vitamin K antagonists: Warfarin
- First-line for strokes caused by valvular atrial fibrillation.
- Novel oral anticoagulants (NOACs):
- Direct thrombin inhibitors (dabigatran) or factor Xa inhibitors (rivaroxaban and apixaban)
- NOACs do not require INR/PT checks and have fewer drug interactions than warfarin.
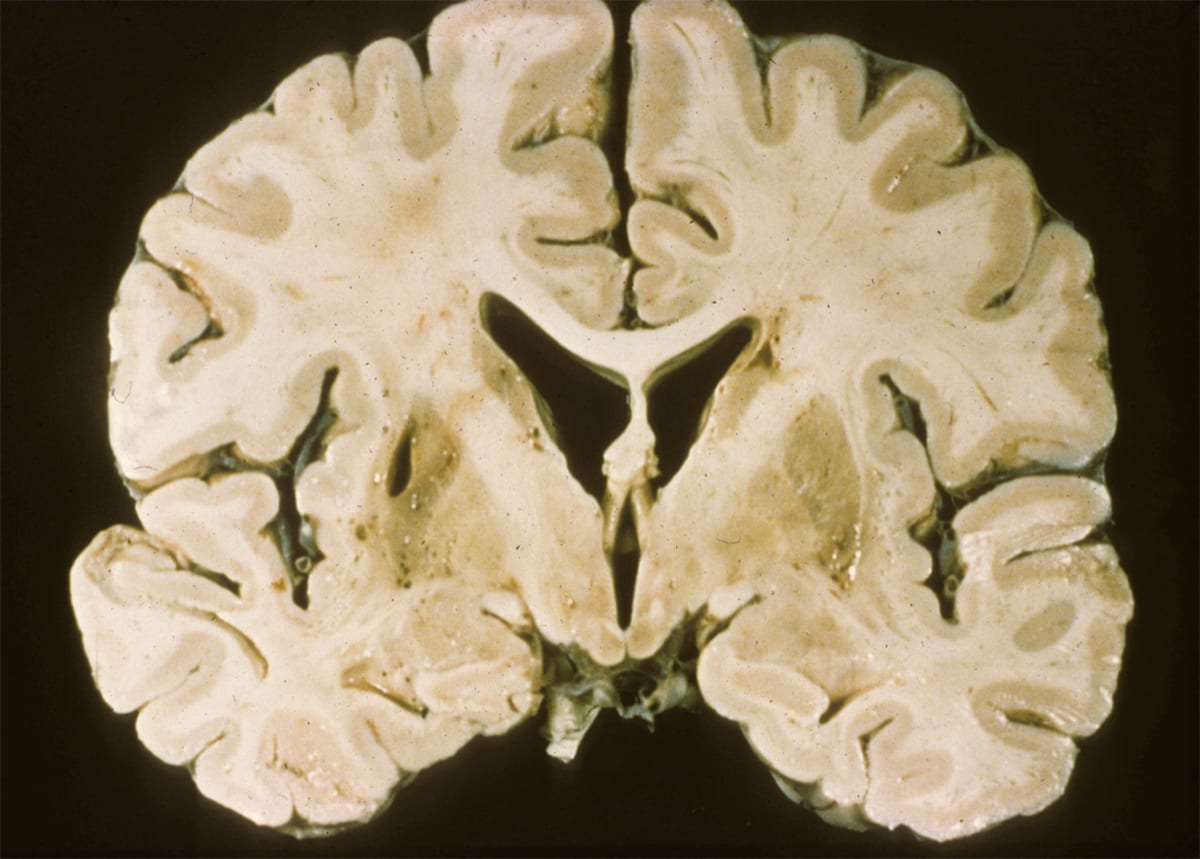
Hemorrhagic Stroke
Intraparenchymal hemorrhage
Causes
- TRAUMA
- Parenchymal contusions are a form of traumatic brain injury where multiple microhemorrhages are found on the interface between brain and bone.
- Patients will often have a concurrent skull or maxillofacial fracture.
- Racoon eyes: Periorbital ecchymoses suggests a fracture of the orbital plate
- Battle sign: Retromastoid ecchymosis suggests a fracture of the petrous portion of the temporal bone.
- Leakage of CSF into the middle ear (CSF otorrhea) or sinus (CSF rhinorrhea) can occur. Samples of leaking fluid can be sent to the lab and tested with beta-2 transferrin assay to distinguish CSF from mucus.
Log in to view the remaining 60-90% of page content!
New here? Choose an account!
1 Month Plan
Full Access Subscription
$68
$
48
49
1 Month -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
3 Month Plan
Full Access Subscription
$159
$
73
49
3 Months -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
1 Year Plan
Full Access Subscription
$446
$
195
49
1 Year -
Access to all chapters
-
Access to all images and cases
-
Access to all flashcards
-
Access to Full Question Bank
Popular
Loading table of contents...
Loading table of contents...